Abstract
Introduction: infections are a significant cause of morbidity and mortality in patients with Multiple Myeloma (MM). In Latin America, data on infectious complications in this patient population are lacking. Recommendations for antibacterial prophylaxis during current standard treatment are heterogeneous. Identifying risk factors for their development would help to define risk-adapted prophylactic strategies.
Methods: We conducted a prospective cohort study of newly-diagnosed MM (NDMM) patients evaluated in 6 Latin American countries between June 2019 and May 2020. Patients must have had active disease and be on active therapy, and with a minimal follow-up of 6 months from the time of diagnosis. Our primary endpoints were to describe the epidemiology of infection events that required hospitalization for more than 24 hours, and to identify risk factors for their development. A logistic regression approach was used to identify the risk factors. In all cases, p < 0.05 was considered significant.
Results: of 248 NDMM patients included in the study, 89 (35.9%) had infectious complications, 21 (23.6%) had 2 or more infectious events (113 infectious episodes), the majority (76/113, 67.3%) occurring in the first 3 months after diagnosis, with the highest frequency in the first month (53/113, 46.9%).
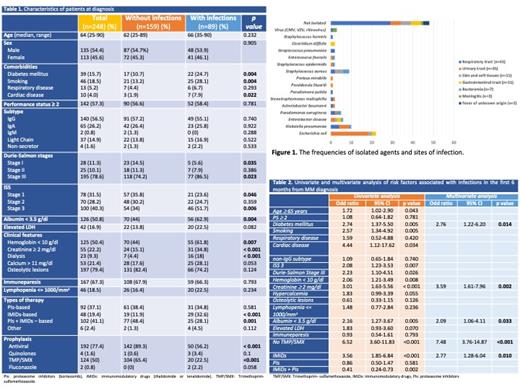
Patients experiencing infections had more frequently Durie-Salmon stage III (86.5% vs 74.2%, p=0.023), ISS 3 stage (51.7% vs 34%, p=0.006), anemia (61.8% vs 44%, p=0.007), renal impairment (34.4% vs 15.1%, p<0.001) and albumin < 3.5 g/dl (62.9% vs 44%, p=0.004). The frequency of infections occurred in 60.4%, 33.7%. and 24.5% in the groups treated with therapy based on immunomodulatory drugs (IMiDs), proteasome inhibitors (PIs) and PIs+IMiDs; respectively (p<0.001). Characteristics of patients and treatments are shown in Table 1.
The most common sites of infection were respiratory (38%) and urinary tracts (31%). In 65 (57.5%) cases, the microbial agent was identified, in 6 cases more than one pathogen was found. Bacterial infections represented 97.3% of the episodes, with Gram-negative bacteria being the most common pathogens (73.5%). Viral infections were infrequent, and no cases of fungal infection were detected. The frequencies of isolated agents and sites of infection are shown in Figure 1.
In multivariable analysis, history of diabetes (OR 2.76, p=0.014), creatinine >= 2 mg/dl (OR 3.59, p=0.002), serum albumin <3.5g/dl (OR 2.09, p=0.033), no use of trimethoprim-sulfamethoxazole prophylaxis (OR 7.58, p<0.001), and treatment with IMiDs (OR 2.77, p=0.010) were independent factors associated to bacterial infections (Table 2).
Overall, 18.6% (21/113) of infectious episodes resulted in intensive care unit admission. Mortality rate at 6 months was 8.5%, and 47.6% of these deaths were infection-related.
Conclusions: We identified infections as a substantial cause of hospital admissions and early death in NDMM patients. Presence of diabetes, renal impairment, low serum albumin and the use of IMiDs were all negative prognostic factors. A risk-adapted approach using the above data will be implemented at the participating centers to reduce infectious complications in NDMM.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal